Medical malpractice cases involving a stroke can be a challenge. Stroke cases are difficult to prove. Are there viable cases? Absolutely. On this page, we will look at medical malpractice cases involving stroke diagnostic errors and the average settlement value of these cases.
This post is for lawyers who are getting stroke misdiagnosis cases but do not know whether the claim is viable. There are common threads that run through the most successful stroke misdiagnosis/failure to treat cases. Cases that result in a settlement or a jury verdict for the plaintiff are usually one of these two breeds: Failing to prevent a stroke and failing to treat a stroke once it has occurred.
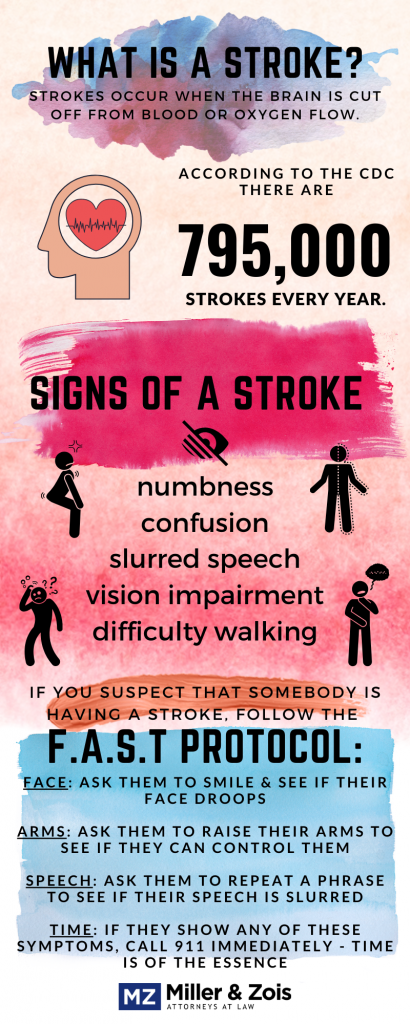
What is a stroke?
Strokes and other cerebrovascular diseases are the third leading cause of death in the U.S. behind heart disease and cancer. A stroke is an interference of the normal circulation of blood flow to the brain. The circulation can be disturbed by a clot or a hemorrhagic process. The latter involves blood leaving the blood vessel and traveling to the space surrounding the brain or inside the brain substance (intracerebral hemorrhage). There are also cases where the clot forms in the cerebral veins, causing cerebral venous thrombosis.
Approximately 7 out of 8 strokes are ischemic. This means there is a lack of blood flow to the brain. This is usually from obstruction from a blood clot or narrowed or closed artery. The most common cause of stroke is atherothrombosis – the combination of atherosclerosis with superimposed thromboembolism (clot) arising from the precerebral and cerebral vessels.
Failing to prevent a stroke malpractice claims
 These kinds of stroke cases involve patients at high risk of stroke because of high blood pressure, atrial fibrillation, diabetes, etc. Many of these patients should be on Coumadin, Plavix, or Heparin.
These kinds of stroke cases involve patients at high risk of stroke because of high blood pressure, atrial fibrillation, diabetes, etc. Many of these patients should be on Coumadin, Plavix, or Heparin.
When evaluating a stroke case, you always want to ask if the patient was on one of these medications before the stroke and if the medication was altered before a stroke. For instance, for certain dental procedures, some dentists will tell a patient to stop taking Coumadin 5 days before the procedure. This subjects the patient to a higher risk of stroke. This might be a viable case.
Some patients have to be bridged, meaning they need to stop Coumadin 5 days prior to the procedure and take a dose of heparin and then titrate back on Coumadin following the procedure. If the stroke happened during this period, it might be a case, if the proper bridging protocol was not followed. Keep in mind, just because a stroke occurs doesn’t mean there was malpractice. Sometimes the protocol is correct, and a stroke occurs, anyway.
A stroke during surgery claim, absent these types of extenuating factors, is a very challenging medical negligence stroke case although sometimes the failure to properly clear the patient for surgery creates a potential claim.
Failing to treat a stroke once it has occurred malpractice claims
The most common stroke malpractice lawsuit is failure to diagnose and treat the stroke. Once a stroke is occurring, there is a brief window for treatment. Many stroke malpractice cases won by doctors and hospitals are because the jury finds that even if there was negligence, it was too late to save the patient from harm or death. Successful treatment depends upon the location of the clot. Certain locations in the brain, for instance, are not easily reached, even with the best clot-buster medication.
Once a stroke is occurring, Coumadin or Heparin cannot dissolve the clot. It can merely prevent future clots. Clot busters sometimes are effective, sometimes not. As a result, these cases are difficult to prove. A typical fact pattern you might see from a caller is a patient who had a stroke, got to the hospital, and was administered a clot buster.
For a time, it looked like they were getting better, but then the next morning they decompensated and now cannot walk or talk. Be careful with cases like these. The damage from a clot sometimes does not manifest itself until several hours after the damage has occurred.
Therefore, it might seem like the patient is better when they really are not. These kinds of cases are very rarely malpractice. Also, sometimes there are cases where a patient is having multiple clots. Sometimes these cases are not preventable, even with Coumadin and/or Heparin.
Four Common Medical Errors Leading to Stroke Malpractice
Stroke-related medical malpractice lawsuits often arise from critical errors in diagnosing or treating patients who are at risk of or actively experiencing a stroke. These cases frequently hinge on preventable mistakes or lapses in judgment that lead to severe and often irreversible harm. Below are the four most common types of stroke malpractice lawsuits.
Misdiagnosis in the ER
Emergency rooms are often the first point of contact for stroke patients. Unfortunately, stroke symptoms such as dizziness, headache, numbness, or slurred speech can sometimes be misinterpreted as less severe conditions like anxiety, migraines, or even dehydration. Doctors have to rule out a stroke. This misdiagnosis delays critical interventions that could prevent permanent brain damage or death. Malpractice claims often focus on the failure of ER physicians to recognize stroke symptoms, perform appropriate diagnostic tests, or consult neurologists when the situation demands specialized care.
Delays in Administering tPA or Referring to Specialists
Tissue plasminogen activator (tPA) is a clot-busting drug that can significantly improve outcomes for patients suffering from ischemic strokes. However, this medication must be administered within a narrow window of time—generally four and a half hours after symptoms begin. Delays in diagnosis, ordering necessary imaging, or determining patient eligibility for tPA can lead to devastating consequences. Malpractice lawsuits in these cases often drill down on avoidable delays in doing what needs to be done caused by poor communication, inadequate triage protocols, or understaffed facilities.
Patients who present at a hospital with an ischemic stroke with symptom onset between four and a half hours or less are strong t-PA candidates. For many reasons, doctors and hospitals often make mistakes that lead to delays that could have been avoided.
Inadequate Pre-Surgical Evaluations
Some strokes occur as a result of surgical procedures, particularly when proper preoperative assessments are not conducted. For instance, if a patient has underlying conditions like uncontrolled hypertension or a history of blood clots, failing to recognize and address these risks can lead to stroke during or after surgery. Procedures like carotid endarterectomy or angiography, while intended to improve blood flow, can trigger strokes if not performed with appropriate precautions. These cases often involve allegations of negligence in pre-surgical planning or the failure to provide adequate postoperative monitoring.
Certain patients, such as those with atrial fibrillation, high blood pressure, or a history of transient ischemic attacks (TIAs), are at an elevated risk of stroke. Physicians who fail to recognize these risks and prescribe preventative measures, such as anticoagulants like Coumadin or Heparin, may be liable for malpractice if the patient suffers a stroke. Additionally, errors in adjusting or bridging anticoagulant therapy for surgeries or dental procedures can further elevate stroke risk. Stroke misdiagnosis malpractice lawsuits often argue that a reasonable standard of care would have involved proactive treatment to mitigate these risks.
Secondary to Surgery
Surgeons sometimes precipitate a stroke in an otherwise healthy patients during routine medical procedures. Such interventions may trigger hazardous blood pressure surges or impair healthy blood circulation. Medical malpractice may ensue if surgical errors, which result in blood clotting, hypertension, or other stroke-inducing causes, occur.
Common procedures that are associated with stroke-related malpractice cases include carotid endarterectomy, which ironically may result in a stroke if the surgeon makes an error during the procedure, and angiography and cardiac catheterization, which may dislodge a blood clot or debris that can end up in an artery leading to the brain.
Neonatal strokes malpractice claims
Neonatal strokes are disturbances in the blood supply in the infant’s brain. One cause of a fetal stroke is hypoxia, which is the loss of oxygen that deprives the fetus of oxygen which causes injury to the brain and other vital organs. This can result in permanent brain damage, cognitive and developmental delays, and lifelong disabilities.
Neonatal strokes can occur for a variety of reasons, including fetal distress during delivery, infections in the mother or baby, blood clotting disorders, and other medical conditions.
When neonatal strokes occur, healthcare providers have a duty to recognize the signs and symptoms of stroke and take appropriate action to minimize the damage to the baby’s brain. This may involve rapid transport to a neonatal intensive care unit (NICU), medication to prevent blood clots or seizures, and other supportive care measures. If healthcare providers fail to recognize the signs of a stroke or delay appropriate treatment, they may be liable for malpractice.
If the obstetrician or midwife failed to see the symptoms of hypoxia and did not take action to head off a stroke, this can be a cause for a viable birth injury claim on behalf of the child and her parents.
Stroke Malpractice Settlements and Verdicts and Settlements
Below are stroke-related malpractice verdicts and settlements. You can find here more stroke malpractice settlements.
2024 Pennsylvania – $400,000 Settlement: 12 days after seeking treatment in 2 different hospital emergency rooms, a 45-year-old woman died from suffered cerebral venous sinus thrombosis (CVST), a brain hemorrhage and catastrophic stroke. Her condition reportedly deteriorated. The wrongful death lawsuit alleged that the ER doctors were negligent in failing to diagnose the CVST which ultimately led to the catastrophic stroke.
2024 Washington – $10,906,000 Verdict: The plaintiff, a 34-year-old female and mother, sought chiropractic care from the defendant for neck pain, back pain, and headaches from a motor vehicle collision. During her treatment, she had the onset of new symptoms, including in her right ear, followed by intense headaches that waxed and waned, dizziness, lightheadedness and vertigo. Soon after, the plaintiff suffered a cerebellar stroke leaving her with permanent impairments. The lawsuit alleged that the defendant was negligent in failing to recognize and diagnose her symptoms and intervene.
2023 Pennsylvania – $4,000,000 Settlement: a 64-year-old woman with a history of multiple stroke risk factors, reportedly underwent elective left lower lobectomy for treatment of early-stage non-small cell lung cancer. 2 days after the surgery she allegedly showed worrisome neurological symptoms and was diagnosed as having suffered a severe stroke. She died a few days after. The lawsuit alleged that the defendants were negligent in failing to timely administer tPA or perform endovascular and/or surgical interventions, and failed to initiate stroke protocol when the decedent was observed with new-onset neurological deficits.
2022 Georgia – $1,500,000 Settlement: Plaintiff suffered a stroke and cognitive damage while recovering from surgery at VA Medical Center in Atlanta. Her stroke malpractice lawsuit alleged that the hospital and doctors were negligent in failing to timely and properly provide brain imaging, complete a cardio-embolic workup or diagnose stroke and failing to train and supervise staff.
2021 Ohio – $250,000 Settlement: A 72-year-old woman underwent a pulmonary biopsy. During the procedure, she became hypotensive. The woman suffered a post-operative stroke. She was left with temporary left leg paralysis. The woman also had limited left arm use and speech deficits. She spent several months in a rehabilitation facility and an assisted living center. The woman’s speech deficits resolved. She also regained some left leg use. However, the woman experienced left arm weakness. She used a cane for ambulation. The woman died from a pre-existing heart condition. Her husband hired an attorney who filed a wrongful death lawsuit against the hospital. She claimed its anesthesiologist and nurse anesthetist failed to control the woman’s blood pressure.
2020 Pennsylvania – $2,500,000 Settlement: A 55-year-old man suffered right-sided weakness, speech difficulties, and dysarthria. The man’s subsequent MRI revealed acute infarction in his middle cerebral artery. He underwent a cerebral angiography that showed severe stenosis. However, the man displayed no neurological deficits, limb weakness, gait abnormalities, numbness, tingling, or speech deficits. This prompted the hospital staff to not diagnose him with a stroke. The man underwent a stent placement. A post-surgical CT scan revealed dense material in his brain. The surgical staff suspected cerebral hemorrhaging. A subsequent arteriogram revealed a large parenchymal hemorrhage. The man became brain-dead several days later. His family alleged that the hospital staff’s negligence caused his death. They claimed they failed to properly diagnose his stroke and order additional tests.
2020 Washington – $18,000,000 Settlement: A 61-year-old woman suffered a severe headache. She presented to the hospital. The radiologist interpreted the woman’s brain MRI as normal and discharged her. Several weeks later imaging revealed a severe hemorrhagic stroke. The woman was left with significant cognitive impairments, partial paralysis, and limb impairments with recurring spasticity. She now required round-the-clock care. The woman alleged negligence against the hospital. She claimed its staff failed to timely diagnose a stroke, properly interpret her brain MRI, and order additional tests.
2019 Texas – $684,000 Verdict: A 74-year-old woman’s physician changed her medication from Pradaxa to Warfarin. Three weeks into taking Warfarin, the woman developed a right facial droop and aphasia. She immediately presented to the emergency room, where she was diagnosed with an ischemic stroke. The woman died the following day. Her surviving relatives alleged that the physician negligently changed her prescription by failing to properly test, diagnose, and treat her anticoagulation levels. They argued that proper testing would have determined that Warfarin increased her stroke risk.
2019 Florida – $875,000 Settlement: A man presented to the ER with numbness to his left side, headaches, and slurred speech. He suspected a stroke. The attending physician ordered a CT scan, which revealed no intracranial issues. He diagnosed the man with heat exhaustion and an anxiety attack, then discharged him home. The following day, the man visited another hospital’s ER, where he was diagnosed with a stroke. He and his wife alleged that the first emergency room delayed his stroke diagnosis by failing to consult a neurologist and failing to appreciate his stroke signs. They also alleged that his delayed diagnosis caused him to suffer permanent paralysis and a severe brain injury.
2016 Oregon – $3,720,000 Verdict: A woman was brought to the ER after she collapsed and lost consciousness at home. The ER physician diagnosed her with emotional problems, prescribed her Ativan, and discharged her home. She subsequently suffered a stroke that led to permanent injuries to her central nervous system and brain. The woman alleged that the ER physician failed to properly diagnose and treat her for a stroke. She claimed that he failed to timely administer tPA, a clot-buster medication, and failed to seek a neurological consultation. The ER physician denied liability, arguing that she appeared to show no signs of a blood clot when she arrived at the ER. A jury awarded the woman $3,720,000, comprising $1,000,000 in medical expenses and $2,720,000 in pain and suffering.
Getting a lawyer for stroke malpractice lawsuit
If you are a Maryland malpractice lawyer and are still struggling to figure out if you have a claim or if you are a victim with a potential lawsuit, call our stroke attorneys (410) 779-4600 or get a free online consultation here.
More information
- Report of a jury verdict in a TIA/stroke misdiagnosis case with links to several stroke misdiagnosis lawsuits filed in Maryland
- Haslett, J. et. al. (2019). Systematic Review of Malpractice Litigation in the Diagnosis and Treatment of Acute Stroke. Stroke, 50, 2858-2864. doi: 10.1161/STROKEAHA.119.025352 This article analyzes medical malpractice cases related to the emergency management of stroke. The study found that allegations which commonly resulted in a payout included failure to timely transfer to another hospital and cases in which the defendant was also negligent in the performance of a surgical procedure that caused the stroke alongside their failure to subsequently timely diagnose/treat it. The study also found that the average payout increased as injury severity increased and that cases involving thrombectomy and failure to treat with tPA were likely to increase. The article highlights the critical role of factors other than adhering to medical evidence in determining the outcome of a legal case.
- How Maryland malpractice lawsuits work
 Maryland Injury Law Center
Maryland Injury Law Center

